What is Chondroplasty?
Chondroplasty is a surgical procedure to repair and reshape damaged cartilage in a joint. The procedure involves smoothing degenerative cartilage and trimming any unstable flaps of cartilage.
Indications for Chondroplasty
Chondroplasty may be recommended if you have mild to moderate cartilage wear or a cartilage injury in your joint, rather than widespread or irreparable cartilage damage. Typically, damaged cartilage does not heal on its own as it does not have a proper blood supply. Medical intervention is necessary to correct the condition. Chondroplasty prepares the joint for further cartilage restorative procedures.
Chondroplasty Procedure
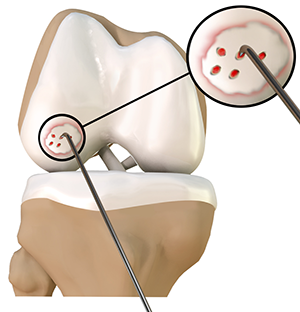
Chondroplasty is a surgical treatment for damaged joint cartilage. It is usually performed by a minimally invasive procedure called arthroscopy.
During the procedure, your surgeon:
- Makes small incisions around your knee
- Inserts an arthroscope (narrow illuminated tube with a camera) which provides an enlarged view of the inside of the joint on a monitor
- Pumps fluid into the joint which expands it to improve visualization
- Uses special tools to remove frayed cartilage or loose fragments
- Trims the damaged cartilage and smoothes the remaining surface
- Drains out the added fluid once the repair is complete
- Closes the incisions with stitches to complete the procedure
Recovery from Chondroplasty
Though you may need crutches or other assistance after chondroplasty, you can usually return to normal activities within three weeks.
Benefits of Chondroplasty
Potential benefits of chondroplasty include:
- Reduced joint pain
- Improved joint function
- Slows cartilage degeneration
- Fast recovery and immediate relief
- Repair or treatment of other abnormalities can also be performed during arthroscopy
Risks Associated with Chondroplasty
The above benefits apart, instances of slight risks such as scarring, or mild pain have been reported.
Related Topics:
- Knee Arthroscopy
- ACL Reconstruction
- Multiligament Reconstruction of the Knee
- Meniscal Surgery
- Cartilage Restoration
- Orthobiologics
- ACL Reconstruction with Patellar Tendon
- Partial Arthroscopic Meniscectomy
- Saucerization
- Intraarticluar Knee Injection
- Knee Fracture Surgery
- Arthroscopic Debridement
- LPFL Reconstruction
- Tibial Derotational Osteotomy
- Failed Meniscus Repair
- Meniscal Transplantation
- Meniscectomy
- Mosaicplasty
- Posterolateral Corner Reconstruction
- Prior Meniscectomy
- Quadriceps Tendon Repair
- Tibial Eminence Fracture
- Trochleoplasty
- ORIF of the Knee Fracture
- Chondroplasty
- Distal Femoral Osteotomy
- Hamstring Autograft
- Hamstring Allograft
- Viscosupplementation
- Physical Therapy for Knee
- Knee Osteoarthritis
- High Tibial Osteotomy
- Tibial Tubercle Osteotomy
- Patellar Tendon Repair
- Robotic Assisted Partial Knee Surgery
- Distal Realignment Procedures
- PCL Reconstruction
- LCL Reconstruction
- MCL Reconstruction
- Cartilage Replacement
- Bicompartmental Knee Resurfacing
- Autologous Chondrocyte Implantation
- Subchondroplasty
- Partial Meniscectomy
- Transphyseal Surgery
- Partial Transphyseal Surgery
- Medial Patellofemoral Ligament Reconstruction
- ACL Reconstruction Procedure with Hamstring Tendon
- Physeal Sparing Surgery (Anderson's Technique)
- Physeal Sparing Surgery (Micheli-KocherTechnique)
- Combined Hyaluronic Therapy for the Knee
- Matrix Induced Autologous Chondrocyte Implantation (MACI)
- Failed Anterior Cruciate Ligament (ACL) Reconstruction
- Physeal Sparing Reconstruction of the Anterior Cruciate Ligament
- Bone-Patellar Tendon-Bone (BPTB) Autograft
- Bone-Patellar Tendon-Bone (BPTB) Allograft
- Pharmacological Interventions for Knee Injuries
- Arthroscopic Reconstruction of the Knee for Ligament Injuries
