What is Mosaicplasty?
Weight-bearing joints, such as the knee, may develop defects in the articular cartilage (spongy tissue that lines and cushions joints during movement) due to stress, trauma or degenerative disease. This can lead to pain, swelling or locking at the joint. Mosaicplasty is a surgical technique to repair the defect by transplanting healthy bone and cartilage from non-weight bearing areas of the knee. It is indicated to treat small cartilage defects of less than 2 cm in young active adults less than 45 years of age.
Surgical Procedure
The surgery is performed under the following steps:
- Mosaicplasty may be performed under general anesthesia, by open surgery or arthroscopy, a minimally invasive procedure that uses a narrow lighted tube with a camera to provide a clear view of the operating site.
- Depending upon the approach, a single large incision or 2 to 3 smaller incisions are made over the affected joint. The defect is removed using a drill and prepared to receive the grafts.
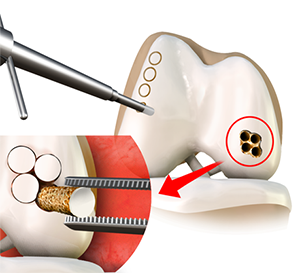
- It is measured to ascertain the number of grafts required to fill the defect. Small healthy cylinders or plugs of osteochondral tissue (cartilage with bone) are harvested from a non-weight-bearing portion of the knee.
- These grafts are inserted into the prepared defect with minimal spacing to fill about 70% of the defect. This allows the body to grow cartilage from the underlying bone and fill in the rest of the defect naturally. The incision(s) are closed.
Recovery after Surgery
Following the surgery, your doctor will prescribe pain medication to keep you comfortable and advise you on limiting or avoiding weight-bearing on your operated leg with the help of crutches. Physical therapy will be introduced to improve range of motion. You will be able to resume your normal activities in 2 to 4 months.
As with all surgical procedures, mosaicplasty may be associated with certain complications such as infection, bleeding, and locking of the joint.
Related Topics:
- Knee Arthroscopy
- ACL Reconstruction
- Multiligament Reconstruction of the Knee
- Meniscal Surgery
- Cartilage Restoration
- Orthobiologics
- ACL Reconstruction with Patellar Tendon
- Partial Arthroscopic Meniscectomy
- Saucerization
- Intraarticluar Knee Injection
- Knee Fracture Surgery
- Arthroscopic Debridement
- LPFL Reconstruction
- Tibial Derotational Osteotomy
- Failed Meniscus Repair
- Meniscal Transplantation
- Meniscectomy
- Mosaicplasty
- Posterolateral Corner Reconstruction
- Prior Meniscectomy
- Quadriceps Tendon Repair
- Tibial Eminence Fracture
- Trochleoplasty
- ORIF of the Knee Fracture
- Chondroplasty
- Distal Femoral Osteotomy
- Hamstring Autograft
- Hamstring Allograft
- Viscosupplementation
- Physical Therapy for Knee
- Knee Osteoarthritis
- High Tibial Osteotomy
- Tibial Tubercle Osteotomy
- Patellar Tendon Repair
- Robotic Assisted Partial Knee Surgery
- Distal Realignment Procedures
- PCL Reconstruction
- LCL Reconstruction
- MCL Reconstruction
- Cartilage Replacement
- Bicompartmental Knee Resurfacing
- Autologous Chondrocyte Implantation
- Subchondroplasty
- Partial Meniscectomy
- Transphyseal Surgery
- Partial Transphyseal Surgery
- Medial Patellofemoral Ligament Reconstruction
- ACL Reconstruction Procedure with Hamstring Tendon
- Physeal Sparing Surgery (Anderson's Technique)
- Physeal Sparing Surgery (Micheli-KocherTechnique)
- Combined Hyaluronic Therapy for the Knee
- Matrix Induced Autologous Chondrocyte Implantation (MACI)
- Failed Anterior Cruciate Ligament (ACL) Reconstruction
- Physeal Sparing Reconstruction of the Anterior Cruciate Ligament
- Bone-Patellar Tendon-Bone (BPTB) Autograft
- Bone-Patellar Tendon-Bone (BPTB) Allograft
- Pharmacological Interventions for Knee Injuries
- Arthroscopic Reconstruction of the Knee for Ligament Injuries
